Sleep is not merely a period of rest—it's an active physiological process essential for cardiovascular health and overall well-being. In recent years, research has increasingly highlighted the profound connection between sleep quality and heart health. This article explores how sleep affects your cardiovascular system, the risks associated with poor sleep, and evidence-based strategies to improve your sleep for better heart health.
The Sleep-Heart Connection: What Science Tells Us
Sleep affects virtually every aspect of cardiovascular function. During normal, healthy sleep, your body undergoes important restorative processes:
- Your heart rate decreases
- Blood pressure drops by 10-20% (known as "nocturnal dipping")
- Inflammation levels are regulated
- Stress hormones like cortisol decrease
- Blood vessel repair mechanisms activate
- Metabolic processes are regulated
These natural rhythms allow your cardiovascular system to recover from daily stressors. When sleep is disrupted or insufficient, these restorative processes are compromised, creating a cascade of physiological changes that can negatively impact heart health.
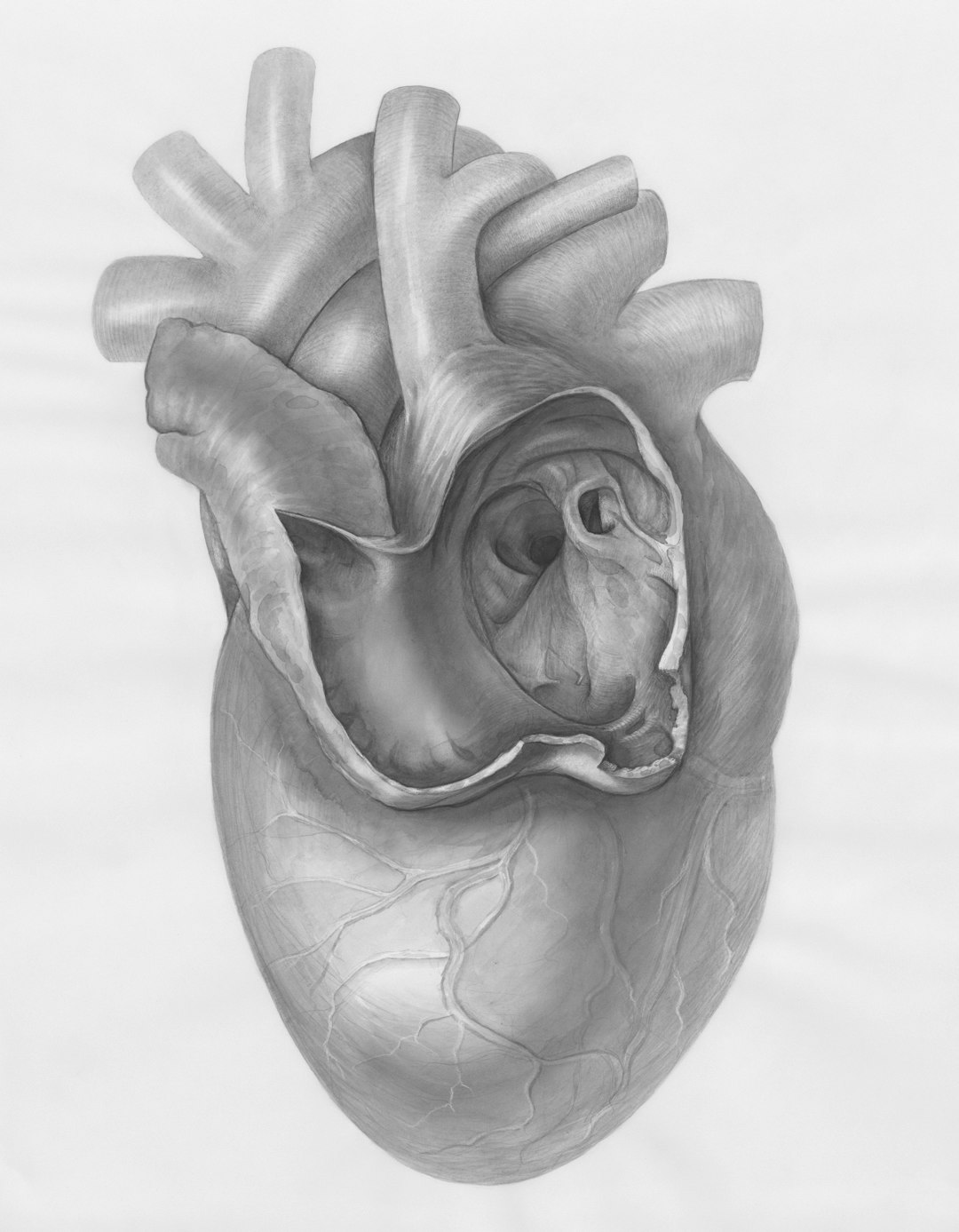
During healthy sleep, heart rate and blood pressure naturally decrease, giving the cardiovascular system essential recovery time.
How Poor Sleep Affects Cardiovascular Health
Multiple aspects of inadequate sleep contribute to cardiovascular risk:
1. Disrupted Blood Pressure Regulation
One of the most immediate effects of poor sleep is on blood pressure regulation. During normal sleep, blood pressure naturally dips by 10-20%. This "nocturnal dipping" is essential for cardiovascular health. Research shows that:
- People who don't experience this nocturnal dip ("non-dippers") have significantly higher cardiovascular risk
- Even a single night of poor sleep can elevate daytime blood pressure
- Chronic sleep deprivation is associated with sustained hypertension
- Sleep fragmentation (frequent brief awakenings) disrupts the normal blood pressure patterns even if total sleep time seems adequate
2. Increased Inflammation
Sleep plays a crucial role in regulating inflammatory processes. Poor sleep quality triggers increased production of inflammatory markers including:
- C-reactive protein (CRP)
- Interleukin-6 (IL-6)
- Tumor necrosis factor-alpha (TNF-α)
These inflammatory markers are directly linked to atherosclerosis (plaque buildup in arteries) and increased cardiovascular risk. Even short-term sleep restriction can significantly elevate these inflammatory markers.
3. Endothelial Dysfunction
The endothelium—the inner lining of blood vessels—is particularly vulnerable to sleep disruption. Research demonstrates that poor sleep:
- Impairs endothelial function, reducing the ability of blood vessels to dilate properly
- Decreases nitric oxide production, a key molecule in vascular health
- Increases oxidative stress, damaging blood vessel walls
- Accelerates endothelial aging and dysfunction
These effects can occur after just a few nights of inadequate sleep and become more pronounced with chronic sleep issues.
Research Spotlight
A 2019 study published in the Journal of the American College of Cardiology found that even healthy adults who were restricted to 5 hours of sleep per night for 8 days showed significant endothelial dysfunction comparable to levels seen in some people with cardiovascular disease.
4. Metabolic Dysregulation
Sleep disruption significantly impacts metabolic processes closely tied to heart health:
- Insulin resistance increases, raising the risk of type 2 diabetes (a major cardiovascular risk factor)
- Appetite-regulating hormones (leptin and ghrelin) become imbalanced, often leading to increased caloric intake and weight gain
- Glucose metabolism is impaired, with elevated blood sugar levels
- Lipid metabolism changes, potentially increasing cholesterol levels
These metabolic changes create a perfect storm for cardiovascular risk, especially when sleep problems become chronic.
5. Autonomic Nervous System Imbalance
Sleep quality directly affects your autonomic nervous system balance. Poor sleep typically leads to:
- Increased sympathetic ("fight-or-flight") nervous system activity
- Decreased parasympathetic ("rest-and-digest") nervous system activity
- Reduced heart rate variability (a marker of cardiac health)
- Increased electrical instability of the heart
This autonomic imbalance creates a state of physiological stress that strains the cardiovascular system and may increase arrhythmia risk.
Sleep Disorders and Heart Health
Beyond general poor sleep quality, specific sleep disorders have strong links to cardiovascular disease:
Obstructive Sleep Apnea (OSA)
OSA has perhaps the strongest connection to cardiovascular disease of any sleep disorder. This condition, characterized by repeated breathing interruptions during sleep, affects an estimated 24% of men and 9% of women. It significantly increases the risk of:
- Hypertension
- Coronary artery disease
- Heart failure
- Atrial fibrillation
- Stroke
- Sudden cardiac death
The good news is that effective treatment of OSA, typically with continuous positive airway pressure (CPAP) therapy, can significantly reduce these cardiovascular risks.
Warning Signs of Sleep Apnea
Common symptoms include loud snoring, observed breathing pauses during sleep, gasping or choking during sleep, morning headaches, excessive daytime sleepiness, and difficulty concentrating. If you experience these symptoms, consult with a healthcare provider, as untreated sleep apnea significantly increases cardiovascular risk.
Insomnia
Chronic insomnia—difficulty falling asleep, staying asleep, or experiencing non-restorative sleep—is independently associated with:
- Increased risk of hypertension
- Higher rates of coronary heart disease
- Greater risk of heart failure
- Elevated stroke risk
These associations remain significant even after controlling for other risk factors, suggesting that insomnia itself contributes to cardiovascular risk.
Restless Legs Syndrome (RLS)
This neurological disorder characterized by an irresistible urge to move the legs, particularly at night, is associated with:
- Higher prevalence of coronary artery disease
- Increased hypertension risk
- Greater risk of stroke
The exact mechanisms linking RLS to cardiovascular disease are still being investigated, but may involve autonomic dysfunction and interrupted sleep.
The Importance of Sleep Duration and Quality
Both sleep quantity and quality matter for heart health:
Sleep Duration
Research consistently shows a U-shaped relationship between sleep duration and cardiovascular risk, with both too little and too much sleep associated with higher risk:
- Short sleep (less than 7 hours): Associated with a 13-24% increased risk of coronary heart disease
- Optimal sleep (7-8 hours): Linked with the lowest cardiovascular risk
- Long sleep (more than 9 hours): Associated with a 30-41% increased risk of coronary heart disease and stroke
While the mechanisms behind the long sleep association are less clear (and may partly reflect underlying health conditions), the dangers of short sleep are well-established.

The relationship between sleep duration and cardiovascular risk follows a U-shaped curve, with 7-8 hours associated with lowest risk.
Sleep Quality
Beyond duration, sleep quality parameters significantly impact heart health:
- Sleep continuity: Fragmented sleep with frequent awakenings increases cardiovascular risk
- Sleep efficiency: The percentage of time in bed actually spent sleeping affects heart health
- Sleep timing: Irregular sleep schedules and circadian disruption negatively impact cardiovascular function
- Sleep architecture: Reduced deep sleep (slow-wave sleep) is associated with higher blood pressure and cardiovascular risk
In some studies, sleep quality measures have proven even more predictive of cardiovascular outcomes than sleep duration alone.
Evidence-Based Strategies for Better Sleep and Heart Health
Improving your sleep can have significant benefits for your cardiovascular system. Here are research-backed approaches:
1. Establish Consistent Sleep Timing
Maintaining regular sleep-wake schedules helps regulate your body's internal clock:
- Go to bed and wake up at the same times daily, even on weekends
- Aim for 7-8 hours of sleep for optimal cardiovascular benefit
- Avoid shifting your sleep schedule by more than an hour, even on days off
- If you need to adjust your schedule, do so gradually (15-minute increments)
2. Create an Optimal Sleep Environment
Your sleeping space significantly impacts sleep quality:
- Temperature: Keep your bedroom cool (65-68°F/18-20°C is optimal for most people)
- Light: Eliminate light sources, including using blackout curtains and removing electronics with LEDs
- Sound: Minimize noise disruptions; consider using a white noise machine if needed
- Comfort: Invest in a supportive mattress and pillows appropriate for your sleeping position
- Electronics: Remove TVs, computers, and phones from the bedroom
3. Develop a Wind-Down Routine
A consistent pre-sleep routine signals your body to prepare for rest:
- Begin 30-60 minutes before your intended bedtime
- Avoid screens (phones, tablets, computers, TV) due to blue light's melatonin-suppressing effects
- Engage in relaxing activities: reading (print books), gentle stretching, meditation, or a warm bath
- Keep lights dim during this time to promote natural melatonin production
- Consider a brief gratitude practice or journaling to reduce anxious thoughts
4. Be Strategic About Light Exposure
Light is the primary regulator of your circadian rhythm:
- Get bright light exposure (preferably sunlight) in the morning
- Maintain good light levels during the day
- Begin reducing light exposure in the evening
- Use amber/red lighting or blue-light blocking glasses 1-2 hours before bed
- Keep the bedroom as dark as possible during sleep
5. Mind Your Consumption Habits
What you consume can significantly impact sleep quality:
- Caffeine: Limit consumption and avoid entirely after 12 PM (or earlier if sensitive)
- Alcohol: While it may help you fall asleep initially, alcohol disrupts sleep architecture and quality
- Large meals: Avoid heavy eating within 3 hours of bedtime
- Fluids: Reduce intake in the evening to minimize nighttime bathroom trips
- Nicotine: Avoid this stimulant, especially in the evening
6. Exercise Appropriately
Physical activity supports both sleep quality and heart health:
- Regular exercise (particularly in the morning or afternoon) improves sleep quality
- Avoid vigorous exercise within 1-2 hours of bedtime, as it can be stimulating
- Consider gentle evening activities like yoga or stretching, which can promote relaxation
- Consistent exercise has been shown to increase deep sleep time
7. Manage Stress and Anxiety
Mental tension is a major sleep disruptor:
- Implement relaxation techniques like progressive muscle relaxation, deep breathing, or meditation
- Consider cognitive-behavioral strategies for managing worries that keep you awake
- Keep a notepad by your bed to jot down thoughts that arise, allowing you to address them tomorrow
- Limit exposure to stressful content (news, work emails) in the evening
The 3-2-1 Rule for Better Sleep
A simple guideline to remember: Stop consuming caffeine 8 hours before bed, alcohol 3 hours before bed, and large meals 2 hours before bed, and put away all screens 1 hour before bed.
8. Know When to Seek Professional Help
Consult a healthcare provider if you experience:
- Persistent difficulty falling or staying asleep
- Excessive daytime sleepiness despite adequate time in bed
- Loud snoring, gasping, or breathing pauses during sleep (as reported by a sleep partner)
- Uncomfortable sensations in your legs that disrupt sleep
- Any sleep problems that impact your daily functioning
Effective treatments exist for most sleep disorders, and addressing these issues can significantly reduce cardiovascular risk.
The Circular Relationship: Heart Health and Sleep
It's important to recognize that the relationship between sleep and cardiovascular health works in both directions. While poor sleep can contribute to heart problems, existing cardiovascular conditions can also disrupt sleep:
- Heart failure may cause breathing difficulties that disrupt sleep
- Cardiovascular medications may have side effects that affect sleep quality
- Chest discomfort from heart conditions can make it difficult to find comfortable sleeping positions
- Anxiety about heart health can contribute to insomnia
This bidirectional relationship can create a vicious cycle, making it all the more important to address both cardiovascular and sleep health simultaneously.
Conclusion: Prioritizing Sleep for Heart Health
The evidence is clear: quality sleep is not a luxury but a necessity for cardiovascular health. Making sleep a priority is one of the most effective lifestyle changes you can make to support your heart.
While nutrition and exercise often receive more attention in heart health discussions, sleep deserves equal consideration. It affects nearly every physiological process relevant to cardiovascular function and interacts with other lifestyle factors to either promote heart health or increase risk.
By implementing the evidence-based strategies outlined in this article, you can improve both your sleep quality and cardiovascular health—a truly heart-smart approach to wellness.